The mortality rate spiked in states with the strictest lockdowns because inner city health care systems are unprepared
07/07/2020 / By Lance D Johnson
During the lock down, the mortality rate in the US for all causes of death went up by five percent, compared to the previous three years. This mortality rate could have been significantly reduced if the inner city hospital systems and nursing homes were more prepared to handle infectious disease outbreaks.
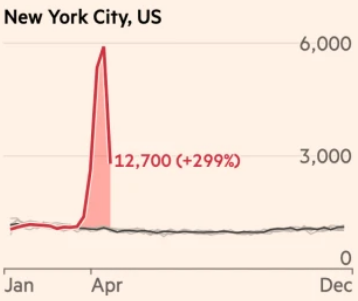
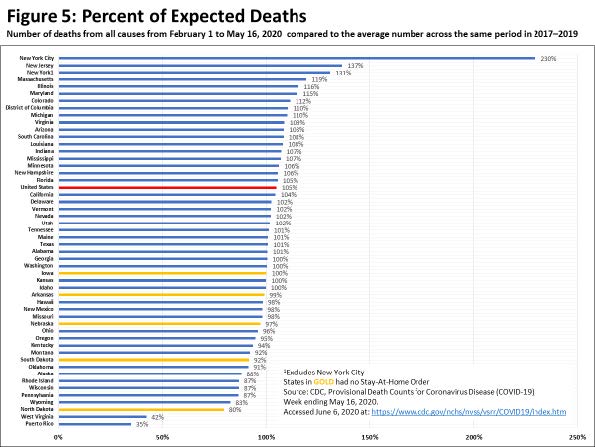
Inner city hospitals are easily overrun, even during a normal influenza season. Nursing homes contain the most vulnerable population, all packed in together, malnourished and pumped full of immune-comprising drugs. These were the catastrophes that occurred primarily in New York City, where the percent of expected deaths was 230 percent from Feb 1 to May 16th.
Fragile inner city health care systems and nursing homes unprepared to face infectious disease
The Cobble Hill Health Center, a 360-bed facility in New York City, lost 55 long term residents very quickly. According to reports, little effort was made to separate elders who had respiratory symptoms from those who did not, and PPE was scarce or misused. “If our governor really wanted to help, he would have first protected the nursing homes,” said resident Mina Clarke. She recalls listening helplessly as her elderly neighbors’ cries for oxygen went unanswered. The CEO of Cobble Hill asked the state for help on several occasions. In an April 9th email he asked, “Is there a way for us to send out suspected covid cases to the Javits center or the ship?” We don’t have the ability to cohort right now based on staffing and we really want to protect our other patients.”
Furthermore, too many patients with respiratory symptoms were rushed onto ventilators and not given anti-viral medications and immune support in order to recover. At Elmhurst hospital in New York City, covid negative patients were put in the same room as covid positive patients, just to save money, and to possibly achieve the financial bonus for getting more positive covid diagnoses. Many patients who were admitted for heart problems, strokes and other chronic diseases and medical emergencies, went on to contract nosocomial covid and pneumonia infections and died on the ventilators.
Other states with the strictest lockdowns had higher than average mortality rates as well. The overall mortality rate jumped in New Jersey (137 percent), Massachusetts (119 percent) and Illinois (117 percent). These states failed to protect the most vulnerable inside their most populated cities. Moreover, the state-wide lockdowns and stay-at-home orders lacked precision, needlessly closing down some businesses in favor of others, unintentionally funneling populations in the places that were allowed to remain open. Controlling and quarantining healthy populations could have contributed to the overall death rate, too, as many lives were burdened by needless changes, restrictions, inter-social and mental challenges, and life stresses that can weaken immune system function.
States with no stay-at-home order were better focused on protecting the most vulnerable
The states with no stay-at-home order had a mortality rate that was lower than expected, compared to the previous three years. Iowa (100 percent) Arkansas (99 percent) Nebraska (97 percent) South Dakota (92 percent) and North Dakota (80 percent) did not mandate that the general population stay home and quarantine. These states did not suspend individual liberties and counted on citizens to use common sense. These states are more rural, less populated, and might be more prepared to handle outbreaks in their cities.
When you look at the bigger picture of public health, the real problem lies in the inner city hospital and nursing home systems, especially in New York City and Chicago. These systems must be improved if the country is going to survive future infectious disease outbreaks. Financial incentives in the medical and insurance systems do not always prioritize human life. These environments are conducive for infectious disease not only because they are high traffic areas but also because they are the places where individual immune system health is lacking.
No amount of contact tracing or staying at home indefinitely will ever improve human immunity and eradicate the spread of viruses. Virus replication can only be stopped when these infectious organisms are exposed to well-functioning immune systems, with healthy cellular defenses that block viral attachment and viral replication. The mortality rate for covid-19 and other infectious diseases will only go down if the most vulnerable populations are treated with dignity — no financial incentives or political games involved. Our most vulnerable need to be given a healthy environment and the nutrients and antiviral medications their bodies need in order to overcome infection.
Sources include:
Tagged Under: coronavirus, deaths, fatalities, hospitalizations, immune system, infections, infectious disease, inner city hospitals, malnutrition, mortality, mortality rate, nosocomial infections, nursing homes, outbreak, pandemic, preparedness
RECENT NEWS & ARTICLES
Pandemic.News is a fact-based public education website published by Pandemic News Features, LLC.
All content copyright © 2018 by Pandemic News Features, LLC.
Contact Us with Tips or Corrections
All trademarks, registered trademarks and servicemarks mentioned on this site are the property of their respective owners.